5 Questions About Plantar Fasciitis
Plantar Fasciitis is a condition that causes severe heel pain. It’s referred to as policeman’s heel; a moniker attributed to the sore feet of cops walking the mean streets of America. But Plantar Fasciitis affects more than just police officers. Studies indicate the condition impacts more than 1-million Americans alone. But what is it, and more importantly, how do you get rid of the disease once diagnosed?
1-How do I know if the source of my foot pain is Plantar Fasciitis?
Let’s start by identifying symptoms that may lead to a clinical diagnosis of Plantar Fasciitis. I think it’s safe to say; we have all experienced sore feet in one form or another. Spend all day tramping around on unforgiving concrete and tile floors of a large shopping mall during the holidays. By the end of the day, not only has a person lost all hope humanity has any redeeming qualities, but their feet ache. Fortunately, this kind of pain usually clears up with rest and by the next day, it’s business as usual. As for hope in humankind? Well, that may take more time.
Not so with Plantar Fasciitis; the Mayo Clinic lists the following occurrences as possible indications. “A stabbing pain in the bottom of the foot, emanating from the heel. Especially if the pain begins straight away, during the first steps of the day, and eases as the patient continues to move throughout the day. Other signs include heel pain after standing for long periods and increasing pain following exercise” (“Plantar Fasciitis,” 2018).
2-What causes Plantar Fasciitis?
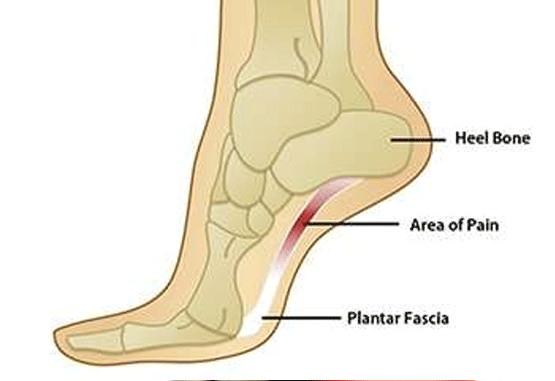
The source of all this pain is a thick sheet of connective tissue covering the bottom of the foot called the Plantar fascia. The tissue is made of collagen and performs a vital function; fascia wraps around muscles and internal organs and serves to stabilizes the entire musculoskeletal system. Think of it as that tough fibrous tape people use to wrap packages. Fascia keeps your flesh from sliding off your bones into a puddle on the floor when you stand up. The Plantar Fascia connects the heel bone to the toes and forms the arch of the foot. The problem begins when the Plantar Fascia becomes stretched. The stretching is a result of the Achilles Tendon, in the back of the foot, contracting and pulling the heel bone. Once stretched, the Plantar Fascia tissue abrades against tiny spurs formed on the heel bone, and the tissue inflames and swells. The resulting pain is Plantar Fasciitis.
3-Who does the disease effect, and why?
With such a large number of Americans diagnosed every year, the causes of the disease are well documented. It should be noted that instances of Plantar Fasciitis can occur without evidence of an underlying cause. But in general men and women between the ages of 40 to 60 with a history of obesity can develop this disorder. In addition to age and weight, another risk group is people with a history of foot problems. The Plantar fascia forms the arch of the foot and those with high-arches or flat-feet are at an increased risk, along with those who have abnormal walking patterns, run long-distances, jump, or perform dance. It’s easy to see why Plantar Fasciitis impacts so many people.
4-What are the treatment options?
Treatment is almost without exception conservative and non-invasive; meaning no surgery is required. But in the interest of full disclosure, there are semi-invasive techniques, short of surgery, your provider may prescribe. For this post, I have limited my discussion to non-invasive treatments only. Please consult a qualified medical provider when considering any treatment option.
In most cases, it will be necessary to see a physical therapist. The therapist will employ a combination of modalities (techniques) proven to get you back on your feet, and pain-free as quickly as possible.
Effective treatment may include the following:
- Weight loss. If excessive weight is a determining factor, then reducing the amount of force body-weight puts on the feet when standing or walking will be critical.
- Manual therapy. A physical therapist will often administer pressure to the lower extremity in the form of deep tissue massage, by hand or with the aid of specialized tools. The use of tools, known as Instrument Assisted Soft Tissue Mobilization, is a recent advancement in treatment and has proven effective at increasing blood flow and promoting healing.
- Exercise and stretching. The therapist will apply specific activities aimed at strengthening and stretching the affected tissue. Home exercise between visits is a vital part of any plan-of-care and will ensure the fastest possible recovery.
- Taping and splinting. Taping supports the muscles of the foot and helps reduce pain. A Dorsal Night Splint may be worn to keep the patient’s toes pointing up, stretching the calf muscle and bottom of the foot while sleeping.
- Icing. The use of an icepack decreases blood flow reducing inflammation and swelling.
- Proper footwear. A therapist can provide examples of footwear designed to promote healing.
- Orthotics. Special foam inserts are designed to support the foot in various ways. Often, inserts can be used right off-the-shelf and are less expensive than a custom version. A therapist might choose to start with the less expensive option, then if necessary, prescribe a custom orthotic in the event option one was unsuccessful.
5-How long will it take to be pain-free?
The answer will depend on three factors, severity of diagnosis, the physical condition of the patient, and the commitment of the patient to achieve a positive outcome. All contribute to the length of recovery. But on average, if working with an experienced therapist, a chronic case could take up to four months to be pain-free while the treatment of an acute diagnosis may take six to eight weeks.
By now, a reader should have a good idea if their symptoms point to Plantar Fasciitis. But that’s not the same as knowing, and only a qualified medical professional can make an accurate diagnosis. To reach a diagnosis, a medical provider will conduct a thorough physical examination and ask questions about the patient’s history and lifestyle. For most providers, this is usually enough to make a qualified diagnosis. On occasion, the examination may include imaging, but this is not considered routine. Regardless, once a definite diagnosis of Plantar Fasciitis is reached, only then can the work of healing begin.
If you have questions or concerns about lower extremity pain including Plantar Fasciitis, talk to a rehabilitation expert at Health Quest Therapy, Inc. Call (907) 376-6363 and schedule your FREE assessment today.
Works Cited
Retrieved from https://www.mayoclinic.org/diseases-conditions/plantar-fasciitis/symptoms-causes/syc-20354846

Very informative. I enjoyed the read.
Thank you for taking a moment to read our blog post.
I really enjoy these posts. I am thankful, however that I don’t have the symptoms.